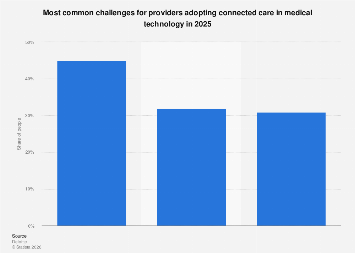
The healthcare industry stands at the precipice of a digital transformation, with connected care solutions promising to revolutionize patient outcomes, streamline operational efficiencies, and enhance accessibility. However, the widespread adoption of these advanced technologies, which encompass remote patient monitoring, telehealth platforms, wearable health trackers, and integrated electronic health records, faces a complex web of significant challenges. As the sector eyes 2025 as a benchmark for increased integration, understanding and proactively addressing these barriers is paramount for realizing the full potential of a digitally empowered healthcare ecosystem.
One of the most formidable obstacles is the persistent issue of data interoperability and standardization. Healthcare systems globally are often a patchwork of disparate legacy systems, proprietary software, and diverse data formats. This fragmentation makes it exceedingly difficult for different connected care devices and platforms to communicate seamlessly and share patient information accurately. Without robust interoperability, the vision of a unified patient record that can be accessed and utilized by various providers and devices remains elusive. This not only hinders effective care coordination but also poses significant risks to patient safety due to incomplete or siloed medical histories. Industry experts emphasize the urgent need for universal data standards and open APIs to facilitate the fluid exchange of information across the healthcare continuum. Organizations like HL7 International are making strides with standards such as FHIR (Fast Healthcare Interoperability Resources), but widespread implementation and adherence across the diverse healthcare landscape are still works in progress.
Cost remains a substantial impediment for many healthcare providers and patients. The initial investment in connected care infrastructure, including hardware, software, and the necessary IT support, can be prohibitive, particularly for smaller clinics, rural hospitals, and healthcare systems in developing economies. Furthermore, the ongoing costs associated with data management, cybersecurity, and maintenance can strain already tight budgets. For patients, the out-of-pocket expenses for wearable devices, subscription fees for monitoring services, and the requirement for reliable internet access can create a digital divide, exacerbating existing health disparities. A study by [Hypothetical Market Research Firm] indicated that while the global telehealth market is projected to reach USD $396.9 billion by 2027, a significant portion of this growth is concentrated in developed nations, highlighting the affordability gap. Governments and insurers play a crucial role in incentivizing adoption through reimbursement policies and subsidies for both providers and patients to bridge this financial chasm.
Patient and provider acceptance and digital literacy represent another critical area of concern. While younger generations may be more amenable to adopting new technologies, a significant portion of the patient population, particularly the elderly or those with limited digital exposure, may struggle with the usability and perceived complexity of connected care tools. Similarly, healthcare professionals, accustomed to traditional workflows, require adequate training and support to confidently integrate these new technologies into their daily practice. A lack of perceived value, concerns about data privacy, and resistance to change can slow down adoption rates. Educational initiatives, user-friendly interface design, and demonstrating the tangible benefits of connected care – such as reduced hospital readmissions and improved chronic disease management – are essential to fostering trust and encouraging widespread uptake. Case studies from early adopters often highlight the importance of change management strategies and continuous user feedback loops in overcoming this resistance.
The evolving regulatory landscape and data privacy concerns present a complex maze for connected care providers. Strict data protection regulations, such as the General Data Protection Regulation (GDPR) in Europe and HIPAA in the United States, mandate robust security measures to safeguard sensitive patient information. Ensuring compliance with these diverse and often stringent regulations across different jurisdictions adds significant complexity and cost to the development and deployment of connected care solutions. Cybersecurity threats, including data breaches and ransomware attacks, are a constant concern, necessitating substantial investment in advanced security protocols and continuous monitoring. Trust is a cornerstone of healthcare, and any perceived or actual compromise of patient data can have devastating consequences for both individuals and the reputation of healthcare organizations. Clearer regulatory frameworks and standardized security best practices are crucial for building confidence and facilitating secure data sharing.
The integration of connected care into existing clinical workflows poses a significant operational challenge. Healthcare professionals are already stretched thin, and the introduction of new technologies can be perceived as an additional burden if not seamlessly integrated. This requires careful redesign of existing processes, efficient data flow management, and ensuring that the technology complements, rather than complicates, the delivery of care. For instance, remote patient monitoring data needs to be easily accessible and actionable by clinicians, without overwhelming them with an unmanageable influx of alerts. Successful integration often involves a phased approach, pilot programs, and close collaboration between technology developers and frontline healthcare staff to ensure that solutions are practical and add genuine value to patient care pathways. The economic impact of inefficient integration can be substantial, leading to wasted resources and reduced productivity.
Furthermore, the need for robust and reliable connectivity, particularly in remote and underserved areas, remains a significant hurdle. Connected care solutions are heavily reliant on stable internet access, both for data transmission and for enabling remote consultations. In many regions, particularly rural communities, the digital infrastructure is inadequate, creating a significant barrier to entry for telehealth and remote monitoring. This digital divide can exacerbate health inequities, leaving those who could benefit most from connected care without access. Investments in expanding broadband infrastructure, exploring alternative connectivity solutions like satellite internet, and developing offline capabilities for certain devices are crucial steps towards ensuring equitable access to digital health services. The economic argument for such infrastructure development is strong, as improved healthcare access can lead to a more productive and healthier population.
The reimbursement landscape for connected care services is still in its nascent stages of development in many parts of the world. While telehealth has seen significant progress in reimbursement policies, particularly following the COVID-19 pandemic, the coverage for other connected care modalities, such as remote patient monitoring for a broader range of conditions, can be inconsistent. This uncertainty can deter providers from investing in and offering these services, as the financial viability is unclear. A more standardized and comprehensive reimbursement framework that reflects the value and cost-effectiveness of connected care solutions is essential to incentivize their widespread adoption. Policymakers and payers are increasingly recognizing the long-term economic benefits of preventative and proactive care enabled by connected technologies, which can lead to reduced hospitalizations and overall healthcare costs.
Looking ahead, the successful widespread adoption of connected care by 2025 hinges on a concerted effort from all stakeholders – technology developers, healthcare providers, policymakers, payers, and patients. Addressing the multifaceted challenges of interoperability, cost, user acceptance, regulatory compliance, workflow integration, connectivity, and reimbursement will require innovative solutions, strategic investments, and a collaborative spirit. The potential rewards of a truly connected healthcare system – improved patient outcomes, enhanced accessibility, and greater efficiency – are immense, but realizing this future demands a proactive and comprehensive approach to overcoming the present obstacles. The economic implications of inaction are also considerable, as lagging in digital health adoption could mean falling behind in global healthcare innovation and efficiency.